A 25 August 2014 “situation assessment” from the World Health Organisation (WHO) noted: “The outbreak of Ebola virus disease in west Africa is unprecedented in many ways, including the high proportion of doctors, nurses, and other health care workers who have been infected. To date, more than 240 health care workers have developed the disease in Guinea, Liberia, Nigeria, and Sierra Leone, and more than 120 have died.”
Rosa Pavanelli, PSI general secretary, called for action. “We cannot accept pitiful excuses, whether from health ministers or donor agencies,” she said. “Health workers must have the tools to do their jobs. All whose work brings them in contact with Ebola victims must have the protective gear. Our members are dying because of unsafe working conditions, this is criminal neglect.”
Médecins Sans Frontières (MSF) said a shortage of trained health workers in Liberia, Sierra Leone and Guinea who can treat Ebola victims and prevent further spread of the deadly disease was hampering response efforts. The agency is shouldering the bulk of the case management burden in the three countries, but is struggling to keep pace with demand. In late August, it said its newly opened Ebola centres in Liberia were “overwhelmed” within days.
Stéphane Doyone, MSF’s West Africa coordinator, said: “We are reaching the breaking point of our capacity where today we can’t guarantee to do more of what we’re doing - particularly when it comes to human resources.” Ebola has no cure, but can be diagnosed and treated. Treatment requires intensive care and close contact between the patient and the healthcare worker.
MSF has deployed 300 health workers, 80 of them expatriate staff, to work on the Ebola response. “It’s a huge programme but human resources are very challenging: staff must be highly trained and they have to be turned over every 4-6 weeks due to stress and fatigue,” said Doyone.
 |
| WORST CASE Health care workers in Africa have died in the ‘worst ever’ Ebola outbreak because they did not have the necessary tools and equipment, according to Public Services International (PSI). It warned in July 2014 that the current Ebola outbreak is “the worst ever and the first to spill widely across several countries.”
|
 |
| EBOLA DEMANDS Dr Ayuba Wabba, the chair of PSI’s West African Health Sector Unions’ Network (WAHSUN), demanded action from Ministries of Health, the World Health Organisation and the West African Health Organisation. “Our unions will keep up the pressure, every day, until our members no longer have to lay down their lives without cause, and until we are able to provide the quality care that is so urgently needed.”
|
 |
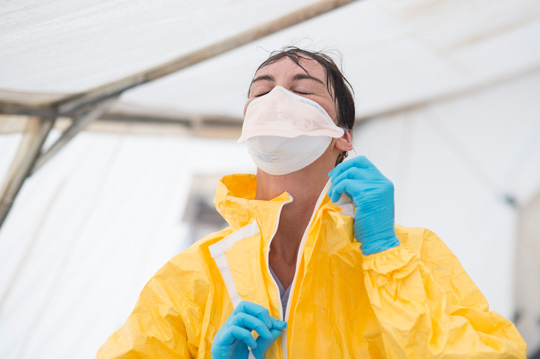
| FEET FIRST When entering or exiting the compound all health care staff must pass a security post to disinfect their footwear and hands. The highest hygiene standards are imperative – over 240 health workers have contracted the virus in this outbreak, and over 120 have died.
|
| CONTAMINATION CONTROL Before entering the isolation ward, staff in this MSF Ebola centre in Guinea pass through dressing rooms where assistants ensure they are wearing protective suits properly. Their gear is sprayed with disinfectant when they leave to ensure nobody contracts the virus while removing the contaminated suit.
|
| SAFETY FIRST MSF has limited its Ebola treatment hospital in Kailahun, Sierra Leone, to 88 beds because safety has to be the “overriding priority”, said Anja Wolz, head of the agency’s operation there. “For us the most important thing is that we're sure about the protection of the staff - from cleaners and drivers to doctors and nurses, and the safety of the patients.”
|
| HIGH PRICE Safety measures in place in MSF’s Kailahun centre in Sierra Leone, where no staff members have died from the disease, involve disposing of up to 5,500 euros’ worth of equipment each day, with the majority of protective suits only worn once.
|
At arm's length

Ebola control efforts and health workers at risk
| Further information | |
| • | Médecins Sans Frontières (MSF) |
| • | Ebola Resource Centre |
| • | Ebola Virus Disease: Occupational Safety and Health - joint WHO/ILO briefing note for workers and employers, Updated 5 September 2014 |
Hazards webpages
Working world • Infections
Images
Click on images for larger versions
All photos: Sylvain Cherkaoui/MSF